There happens to be a group of healthcare professionals and scientists that believe Lyme disease is difficult to catch and easy to cure. Doctors that treat their Lyme patients with courses of antibiotics beyond what is suggested by guidelines are attacked by medical boards and the media in what looks like a coordinated manner.
While patients continue to suffer and end up bed ridden, in a wheelchair or death in extreme cases, some healthcare professionals continue to deny the chronic illnesses that develop after tick bites in many patients around the world. These deniers suggest that patients rather suddenly have developed psychiatric illnesses and actively promote the idea that doctors that are taking care of these patients are trying to take unfair advantage of them.
How did we end up in this complicated, polarized debate and is there truly no line of evidence that suggests that Lyme disease can survive the current antibiotic treatments?
History of Lyme disease
Lyme disease is named after the town Old Lyme in Connecticut. Allen Steere was asked by the Connecticut Department of Health to investigate a mysterious outbreak of juvenile arthritis. He noticed that some of the patients he studied also presented with a red circular rash with central clearing. This rash was later referred to as Erythema Chronicum Migrans. The onset of this mysterious disease seemed to be during spring, summer or early fall. Because of the clustering in specific areas and the seasonal onset of the disease, Steere suspected that the disease was spread through an arthropod insect, probably a tick.
In Europe a similar disease was reported. After a tick bite European scientists described the same chronic skin rash that was accompanied by a long list of strange symptoms involving the heart, skin, joints and central nervous system. In Europe they suspected that this disease was caused by a spirochete because the early stage of this disease responded to treatment with antibiotics. Allen Steere was not convinced. The disease in Connecticut was characterized by arthritis, a relatively unusual phenomenon in European patients.
Steere’s findings emerged rapidly. In 1977 he reported in Annals of Internal Medicine that the disease had an ‘enlarging clinical spectrum’. Arthritis was only one of several possible outcomes after the rash and no longer a strict criterion for the disease. He described a broad spectrum of symptoms: malaise, fatigue, chills and fever, headache, stiff neck, back pain, muscle aches, nausea and vomiting. Within this broad spectrum of symptoms, he identified what he regarded as the most specific signs of the disease: migratory joint pains and neurological and cardiac abnormalities.
While a group of doctors had good results with treating their Lyme patients with antibiotics, the group at Yale held back. Steere thought it was more than justified to ignore the European studies in favor of his clinical observations at Yale. Eight Yale patients had received antibiotics for their Erythema Chronicum Migrans before they were admitted to the study at Yale and despite the antibiotics they developed joint pains, neurological abnormalities and cardiac symptoms. That is why Steere thought that antibiotics would not help.
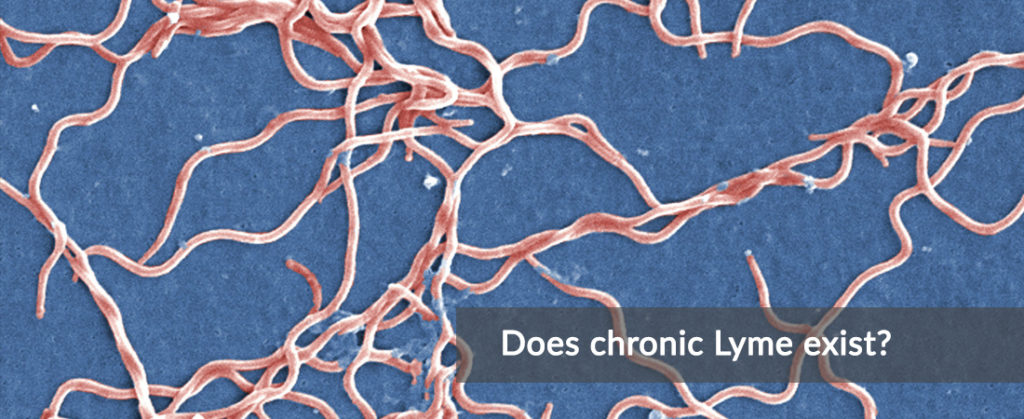
Discovery of the Spirochete
In 1981, while Steere and his team were looking for a virus that could be the possible cause of Lyme disease, microbiologist Willy Burgdorfer was involved in a collaboration with the State of New York in the search for ticks that contained Rocky Mountain Spotted Fever. In October, Jorge Benach and Edward Bosler went to Shelter Island to find ticks containing the pathogen. They collected a batch of Ixodes ticks and sent them to Burgdorfer who would dissect the ticks.
Burgdorfer found no evidence of the bacterium that caused Rocky Mountain Spotted Fever but he did discover that there were spirochetes in the gut of the tick. While observing these micro-organisms he knew he had won the jackpot: he had just discovered the elusive cause of Erythema Chronicum Migrans in Europe and Lyme disease in the United States.
Hours after the discovery, he dissected 124 extra ticks and examined their contents. Sixty percent of the ticks contained the spirochetes. It took a few extra days for Burgdorfer to find the presence of similar spirochetes in the intestines of the European tick, Ixodes ricinus. The related Borrelia species that he found were eventually called Borrelia garinii and Borrelia afzelii and would be known as the causative agents of the European variant of Lyme disease.
Major – Minor
Steere’s first belief that Lyme was viral – and therefore not susceptible to antibiotics – affected the first results that showed that two weeks of antibiotic treatment made almost no difference. In 1981 the discovery of Burgdorfer would shake things up. Lyme disease was a bacterial infectious disease and Steere could no longer ignore it: he could no longer claim antibiotics were ineffective in treating Lyme disease.
Steere went back to the drawing board and in July 1983 he published a new recommendation in Annals of Internal Medicine based on 3 years of data from his first Lyme patients. He tried to determine which of the three antibiotics – penicillin, tetracycline or erythromycin – was the most suitable to cure the Erythema Chronicum Migrans. The researchers treated each patient with antibiotics for ten days. Those in whom the Erythema Chronicum Migrans recurred or continued to grow were retreated with second 10-day course of antibiotics. The patients were then followed to see which of them would progress and develop joint pain or neurological symptoms or the broad picture of other symptoms by which the disease could manifest itself. After analyzing the data, Steere recommended to treat the infection with tetracycline for ten to twenty days.
Those who take a closer look at this study are disturbed: according to Steere’s own data, almost as many patients remained ill as in the previous treatment studies that showed that two weeks of antibiotics were not effective. It was at least remarkable that treatment success was now claimed, while treatment failure was reported earlier – based on the same data.
The answer can be found in the methodology of the study. Steere managed to achieve a higher treatment success by setting a new definition of cure and by reorganizing his data. In his earlier work, before the discovery of the spirochete, Steere had reported that many of his patients developed ‘late manifestations’ of the disease: the joint pains, neurological symptoms and a broad group of symptoms such as headaches and fatigue.
In order to be able to claim treatment success instead of treatment failure, Steere made a strategic adjustment: he divided the late manifestations of the disease into two groups: ‘major’ and ‘minor’. The ‘major’ symptoms of late Lyme were the ‘real’ or objective symptoms. One of the expressions was meningoencephalitis, characterized by a stiff neck, severe headache and increased white blood cells that indicated an infection. Another major symptom was recurrent joint pain with swelling. The minor symptoms consisted of facial paralysis, heart rhythm abnormalities, headaches and joint pain. Fatigue or severe fatigue, confusion and memory loss were labeled as ‘minor’.
Lots of the very disabling but subjective symptoms could be classified as ‘minor’. All these symptoms would be post-infectious or not even related to Lyme disease in Steere’s mind. A patient could end up in a wheelchair, develop a complex seizure-disorder, or have severe pain and fatigue but Steere didn’t think these would respond to further treatment with antibiotics. Unfortunately, this perspective on Lyme disease has even led some patients to threaten Allen Steere with dead.
Animal models
Due to the nature of the Lyme spirochetes, research into persistence after antibiotic treatment was not easy and certain methods that are used on autopsy in animals are simply not usable in human patients. Over time, different animal models have demonstrated that Lyme disease can persist the current treatments. The results of these studies support the idea that persistence also plays a role in human patients who continue to suffer from symptoms after antibiotic treatment.
Straubinger’s Beagles
Reinhard Straubinger is a researcher at Cornell University, New York, who did a study in 1997 with nineteen Beagles. He infected these dogs with Lyme disease by allowing infected ticks to feed on them. Two months later he tested the dogs for Lyme disease. Eighteen of the dogs got infected with the Lyme disease causing spirochete.
Twelve of the dogs got treated with antibiotics and six dogs were left untreated. Eleven of the twelve treated dogs recovered from antibiotic therapy and their antibody response declined. Four of the six untreated dogs went on to develop arthritis. Six months later Reinhard autopsied the dogs. All of the treated dogs showed persistence of spirochetal DNA in their tissues.
Straubinger observed that the antibodies rose consistently over time in the untreated dogs but the antibody response in the treated dogs showed a dip during treatment with antibiotics. Six months after finishing the antibiotic treatment, the antibodies started rising again. Combined with the persistence of spirochetal DNA this suggested that the spirochete survived antibiotic therapy according to Straubinger.
Barthold’s Mice
Stephen Barthold and Emir Hodzic of the University of California Davis did multiple studies on mice.
One of the first studies was done in 2002 with Linda Bockenstedt and Durland Fish, both co-authors of the IDSA Lyme disease guidelines. In this study they found that spirochetes could persist, even 9 months after an antibiotic treatment, but they could not demonstrate the infectivity or pathogenicity of these persisting spirochetes.
In 2008 Stephen Barthold and Emir Hodzic repeated a similar study. They found that one month after antibiotic treatment none of the mice had clinical signs of Lyme disease and cultures could not detect the spirochete. However 3 months later they could transmit living spirochetes from one mouse to uninfected ticks which they could also accomplish by skin graft. Five of the mice examined showed spirochetal DNA in their tissues.
After autopsy they could still find persisting spirochetes in small numbers in collagen rich areas surrounding the heart, tendons and ligaments. It did not matter how fast treatment was given after infection: all mice had persisting spirochetes. These spirochetes were non-dividing but infectious. The researchers could transmit the spirochetes from the infected mice to sterile ticks but they could not grow them in culture.
In a study in 2014, Barthold and Hodzic showed that mice treated with Ceftriaxone had persisting non-cultivable spirochetes in their tissues. DNA was detectable 2, 4 and 8 months after treatment and after 12 months they detected an increase in DNA content.
Despite that these spirochetes remained in a non-cultivable state, the researchers could detect RNA transcription, they could acquire spirochetes by xenodiagnosis and spirochetal forms could be visualized inside the ticks used for xenodiagnosis and in mouse tissues. This suggests that the Lyme disease spirochetes can multiply in ways we cannot culture.
Embers’ Monkeys
In a study from 2012 Monica Embers demonstrates that spirochetes persist in monkeys after 30 days of antibiotic therapy. Antibody response declined in treated animals but Borrelia antigen, DNA and RNA was found in the tissues of the treated monkeys.
Monica Embers found direct evidence of persistence in all monkeys treated with 28 days of antibiotics and in eight out of eleven monkeys treated with the 90 day Klempner protocol – which consists of treatment with Ceftriaxone for 30 days followed by Doxycycline for 60 days.
Gary Wormser had multiple points of criticism on the 2012 study. Monica Embers designed a new study, processed Wormser’s criticism, and demonstrated yet again in 2017 that living spirochetes persist in monkeys after treatment with antibiotics. Intact spirochetes were observed in the brains, the heart and peripheral nerves of the treated monkeys. The study also indicates that immune response varies widely in treated and untreated monkeys.
It is apparent from Embers’ data that these spirochetes have the ability to escape immune recognition, tolerate antibiotics and invade vital organs such as the brain and heart. Antibody tests failed to detect Lyme disease in a number of monkeys with persistent Lyme disease over time, even though Embers found direct evidence of the bacteria which confirmed persistence of the infection.
Laboratory persistence
Prof. Ying Zhang and Prof. Kim Lewis have conducted studies on how Lyme disease spirochetes evade killing by antibiotics in the laboratory. They found that the Lyme spirochetes have different strategies to tolerate antibiotics that are currently used in treatment. The Lyme spirochete Borrelia is a very intriguing and complex organism that changes forms: spirochetal forms, variant round-body forms, aggregated micro-colony forms and even larger biofilm-like structures.
These persisters and dormant cells allows a small population of cells to become specialized survivors. When something unpleasant hits the population like antibiotics, these are going to be the only cells that survive and will cause a chronic, relapsing infection. These dormant forms shut down their metabolism and their targets become inactive. In order to kill a cell, the antibiotic has to corrupt its target, if the target is inactive, there is nothing to corrupt.
In the case of Lyme disease Zhang and Lewis demonstrated that Lyme disease survives antibiotics that have been previously thought to be curative. After the antibiotic is washed out of the culture, the infection grows back.
Zhang explored different antibiotics and combinations. He finally came up with a combination of three drugs: a tetracycline, a cephalosporin and daptomycine. This combination was, in contrast with other antibiotic combinations, able to sterilize the culture without regrowth. This might explain why current antibiotics are not successful in eradicating the infection in animal models and why patients continue to have symptoms.
Intracellular evasion
Besides the ability of Lyme spirochetes to persist antibiotics by going dormant another evasion strategy is that Lyme Borrelia can hide inside of different cells to survive lethal doses of antibiotics. Multiple studies demonstrate that Borrelia can penetrate fibroblasts, endothelial cells, synovial cells, macrophages and B-cells in cell culture and animal models. Miklossy and her colleagues demonstrate how Lyme spirochetes can invade neurons and glial cells in the brains of Lyme patients. She also confirmed that the atypical forms seen in the laboratory also exist inside of infected hosts. A full list of studies demonstrating the ability of Borrelia spirochetes to invade cells is provided in the references.
Fibroblasts
Mark Klempner examined if skin fibroblasts protected the Lyme spirochetes against Ceftriaxone, an antibiotic commonly used to treat Lyme disease. In the presence of fibroblasts the bacteria survived the administration of lethal doses of Ceftriaxone. In the absence of these fibroblasts the organisms did not survive. The fibroblasts protected Borrelia for at least 14 days of exposure to Ceftriaxone. Klempner further demonstrated that a living cell was required to have this protective effect and that other cell types also provided the Lyme disease spirochete with a protective environment.
Endothelial cells
Ma, Sturrock and Weis demonstrated that Lyme spirochetes can invade endothelial cells. 10-25% of the Lyme spirochetes invaded these endothelial cells within 24 hours. Comstock and Thomas observed the same phenomenon on multiple occasions. These scientists conclude that the spirochetes can evade antibiotics and/or the immune response by hiding inside endothelial cells.
Synovial cells
Girschik and his colleagues demonstrate that Lyme spirochetes can invade synovial cells and persist inside of them for at least 8 weeks. Treatment with Ceftriaxone was unable to eradicate the intracellular spirochetes. According to the authors these data suggested that Lyme disease is able to persist within resident joint cells in the host.
Neurons & glial cells
Judith Miklossy and colleagues report that the atypical forms of the Lyme spirochete that are seen in the laboratory also occur inside the host. She also reports that Lyme spirochetes can invade and persist inside glial cells and neurons. This further demonstrates the importance of antibiotics that can penetrate and kill spirochetes inside of cells. It also shows the importance of the work from professor Zhang and Lewis with regards to these atypical and persisting forms of the Lyme spirochete.
Case reports
In the early years of Lyme disease research many scientists were open to the idea that Lyme disease could persist after antibiotic therapy. They were more actively trying to rule out persistent infection in individual cases and groups of patients which led to multiple case reports that demonstrated the reality of persistence. Over the years the debate surrounding Lyme disease became more polarized and physicians stopped ruling out persistence of the infection in patients in favor of a PTLDS label.
One of the cases that demonstrated persistence was presented by Kenneth Liegner. His patient’s case is quite intriguing because his patient was treated with multiple rounds of oral and IV antibiotics, much longer than current guidelines recommend, and despite these prolonged treatments, the CDC could still culture Lyme disease bacteria from the spinal fluid of his patient.
A full list of case reports that demonstrate persistence of Borrelia by culture and/or PCR is provided in the list of references.
Persistence in the eye
Preac-Mursic et al describe six patients in whom Lyme bacteria persist in the eye; demonstrated by the ability to culture spirochetes from iris, skin and cerebrospinal fluid of these patients. In two of the six patients antibodies were negative. This demonstrated that patients may have subclinical or clinical disease without diagnostic antibody titers.
Persistence in joints
A 15 year old girl from Austria was bitten by a tick. She did not develop an Erythema Chronicum Migrans. Three months later she was diagnosed with facial palsy. Repeated serology confirmed Lyme disease and she was treated with two weeks of amoxicillin. She had an adverse reaction, thus treatment was switched and continued with 2 weeks of doxycycline after which residual paralysis of the facial palsy resolved.
Two months later the patient developed arthritis of the knee. Culture for Lyme disease was positive. She was retreated with Ceftriaxone 4 g per day for 3 days after which the treatment was continued with normal doses of 2 g daily for 11 days after which she remained free of symptoms at a 6 month follow up.
Persistence in ligamentous tissue
Haupl and colleagues describe a case that progressed to a chronic stage with multisystem manifestations despite antibiotic therapy . The initial significant immune system activation was followed by a loss of the specific humoral immune response and a decrease in the cellular immune response to Borrelia burgdorferi over the course of the disease. Viable spirochetes were identified from a sample obtained at surgery. The spirochetes were situated between collagen fibers and along fibroblasts, some of which were deeply invaginated by these organisms.
Co-infections
Besides the real possibility that Lyme disease can persist after treatment, there are many more tick-borne infections that can cause ongoing symptoms, that need a different treatment approach and are just as tolerant to treatment as the Lyme spirochete. Babesia and Bartonella are both infectious organisms that can be transmitted by ticks besides or alongside of the causative agent of Lyme disease.
When you contract multiple infections from a tick bite, it is possible that your ongoing symptoms after treatment for Lyme disease are caused by one of these other tick borne infections. Tests for these co-infections are in some cases even more unreliable than the tests currently available for Lyme disease. Much is still unknown in regard to how these co-infections should be treated.
NIH clinical trials
Multiple NIH funded clinical trials showed improvement from repeated antibiotic treatment in patients who had confirmed Lyme disease and were treated with antibiotics before. Brian Fallon, who coordinated one of these clinical trials doesn’t understand why the IDSA, British Infection Association and European Federation of Neurological Societies find it so difficult to see that there is an improvement associated with repeated antibiotic therapy as demonstrated by two of these clinical trials.
Fallon Study
Brian Fallon is the director of the Lyme and Tick-Borne Diseases Research Center at Columbia University. He performed a study in which they assessed the improvement of 10 weeks IV Ceftriaxone compared to 10 weeks of IV placebo in patients with confirmed Lyme disease that were treated before but who had continuous symptoms.
The Fallon study showed improvement in persistent symptoms from repeated antibiotic therapy. Unfortunately these improvements didn’t sustain until the end of the study, twelve weeks after the antibiotic treatment. His study showed that a greater severity of symptoms was associated with greater likelihood of improvement from repeated antibiotic therapy.
Brian Fallon also showed that the pain of patients with chronic symptoms after treatment can be comparable to post-surgical pain, that their fatigue can be comparable to what M.S. patients experience and he compared their level of physical disability to that of patients with congestive heart failure.
Krupp Study
The Krupp study aimed to determine whether PTLDS responds to re-treatment with antibiotics. The outcome measures where fatigue, reaction time and OSP-A in the central spinal fluid of patients. Only the fatigue in these patients was uniformly impaired which means it would be more difficult to show improvements on any of the other outcome measures.
64% of the patients on antibiotics improved in comparison to 18% of the placebo group. This is a significant difference. When you look at the patients that entered the study with a positive IgG Western Blot, the treatment response was even greater: 80%.
The researchers found no difference in cognitive impairment and OSP-A was a meaningless outcome measure since only 9 out of 55 patients had OSP-A in their spinal fluid to begin with. Because only fatigue was uniformly impaired in these patients , the lack of treatment effect in any of the other outcome measures could be expected.
Comparing the Fallon and Krupp Study
The Fallon and Krupp study results are identical in terms of improvement. The effect size for re-treatment was moderate to large. For a lot of conditions the FDA approves drugs with just a mild effect size. Re-treatment with antibiotics for PTLDS had a moderate to large effect size.
It is important to note that these studies only selected patients with homogeneous symptoms. If you design a clinical study, such as the recent PLEASE study, where you look at a wide range of symptoms, and have confusing entrance criteria, you may not be able to show a treatment response. Whereas if you focus on a particular problem based on its severity, you are more likely to demonstrate a treatment effect.
PTLDS
According to current logic you could be in a wheelchair, suffer from debilitating seizures, have continuing cardiac symptoms and suffer from tremendous pain and they would call those “residual symptoms” attributed to a “post-infectious syndrome”; regardless of whether or not these symptoms respond to repeated antibiotic treatment. The treatments that are currently employed to leverage these persistent and debilitating symptoms are inadequate and do not improve the condition of these patients in any meaningful way.
Several lines of evidence demonstrate the validity of the post-infectious concept but at the same time this doesn’t rule out the possibility that this condition can be caused by persistence of the spirochete. For some physicians PTLDS is a euphemism for treatment failure. In a more nuanced context the PTLDS and persistent infection concepts are not mutually exclusive of each other. In practice PTLDS is a rather cruel reality: patients who continue to suffer from debilitating symptoms, with pain comparable to what you might experience post-surgery and physical disability that is equal to that of patients with congestive heart failure are abandoned by healthcare and their government by labeling their chronic symptoms as PTLDS.
Open scientific community
Scientists who come up with research projects to improve understanding of these tick borne illnesses are having difficulty applying for grants. Many of their applications are knocked back with reasons such as: “We do not hand out money to research an imaginary illness.”
My case report
My case report describes how, in my particular case, persistence of Lyme disease was objectively proven by culture and how multiple blood cultures came back positive for Bartonella henselae. It took multiple, repeated courses of antibiotics to cure Lyme disease, as defined by the inability to culture the spirochete from my spinal fluid and blood.
My strain of Bartonella henselae was shown to be naturally resistant to macrolides and had acquired resistance against tetracyclines from earlier therapy targeting Lyme disease. Treatment with fluoroquinolone antibiotics improved all my symptoms that could also be attributed to PTLDS.
My case demonstrates that Bartonella henselae can persist and cause bacteremia for more than 7 years despite multiple courses of antibiotics and that my symptoms that could be attributed to PTLDS, responded to treatment with a fluoroquinolone antibiotic. This suggests that my simultaneous infection with Bartonella henselae is more likely to be the cause of my persistent symptoms than a post-infectious syndrome such as PTLDS.
Gatekeepers
I found it really interesting to come to an understanding that chronic Bartonellosis can present itself with unspecific, subjective symptoms and might overlap with what patients with PTLDS describe. Unfortunately, editorial boards thought differently about that: “It was not medically relevant or interesting.”
Multiple physicians who documented the persistence of the Lyme spirochete in their patients experienced the same rejection. These experiences lead them to believe information is purposely suppressed and denied.
If promising research projects are denied funding and important data is being denied for publication, that might make someone wonder what terms such as ‘data-driven’ and ‘evidence-based’ science mean. The current state of affairs can sometimes give the appearance that there is no open scientific community, as editorial boards and grant review boards could act as gatekeepers to actively protect a very narrow definition of a disease.
Harmful denial?
Different lines of evidence demonstrate persistence in individual cases, animal models and the laboratory. Despite this evidence a small group of healthcare professionals claims that there is no evidence for persistent Lyme infection.
Some of these healthcare professionals who are denying the persistence of Lyme disease after antibiotic therapy are also actively spreading misinformation to mislead the media in a fight against physicians that choose to abandon outdated guidelines and recommendations in individual cases, where patients seem to be benefiting from prolonged and repeated courses of antibiotics.
Come together
A lot of the symptoms that chronic Lyme patients experience are very unspecific and subjective. I don’t doubt these symptoms are real since I have experienced them myself. I understand that this makes it much more difficult to find answers. In the meanwhile I hope patients find ways to cope and treatments to manage their symptoms. Hopefully, physicians helping us will stay open-minded.
Lyme-patients can live with the understanding that there is no turnkey solution but we are done with the semantics, stigmatization, disbelief and misinformation. When you continue to state false facts long enough, they are accepted as truth. This is not only hurtful, it also fuels the way society interacts with patients suffering from chronic Lyme disease. You can learn more about the social consequences of having chronic Lyme disease in an interview I will soon do with Huib Kraaijeveld, a social psychologist with a special interest in Lyme disease.
I hope we can put an end to this harmful debate, have a more nuanced dialogue and come together in an effort to find solutions. In my opinion it is too early to discard persistence of infection completely.
Many Blessings,
CrystalRiver